Peripheral Vascular Disease
This refers to diseases of the blood vessels outside the heart and brain. It is often a narrowing of vessels that carry blood to the legs, arms, stomach or kidneys. There are two types of these circulation disorders
- Functional peripheral vascular diseases don’t have an organic cause. They don’t involve defects in blood vessels’ structure. They’re usually short-term effects related to “spasm” that may come and go. Raynaud’s disease is an example. It can be triggered by cold temperatures, emotional stress, working with vibrating machinery or smoking.
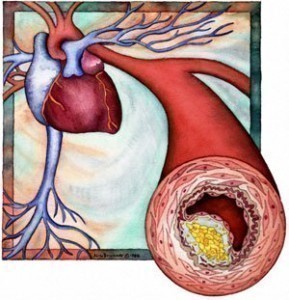
- Organic peripheral vascular diseases are caused by structural changes in the blood vessels, such as inflammation and tissue damage. Peripheral artery disease is an example. It’s caused by fatty buildups in arteries that block normal blood flow.
Peripheral Artery Disease
The Peripheral Artery Disease (PAD) is a condition similar to coronary artery disease and carotid artery disease. In PAD, fatty deposits build up in the inner linings of the artery walls. These blockages restrict blood circulations, mainly in arteries leading to the kidneys, stomach, arms, legs and feet. However, it includes all diseases caused by the obstruction of large arteries in the arms and legs.
Causes of Peripheral Artery Disease
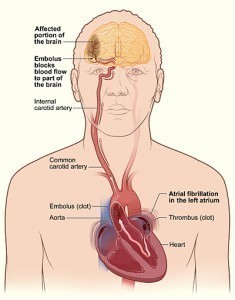
PVD is a result from atherosclerosis, an inflammatory process that leads to stenosis, an embolism or thrombus formation.
Internationally, Smoking of the tobacco is the single most important thing that cause PVD. Smokers are at risk and are prone to be affected. Also exposure to second hand smoke from environmental exposure has also been shown to promote changes in blood vessels lining which is a precursor to atherosclerosis. Other causes include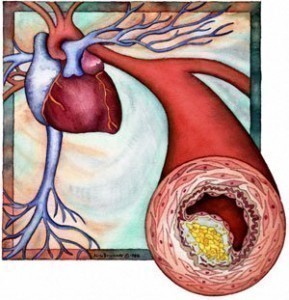
- Diabetes Mellitus
- Dyslipidemia
- Hypertension
Symptoms
- Pain
- Weakness
- Numbness
- Cramping
- Muscles due to decreased blood flow
- Sores
- Wounds
- Ulcers that heal slowly
- Diminished hair and nail growth on affected limb
Treatment
- Physical Exam
- Ultrasound
- X-ray Angiography
- Magnetic Resonance Imaging Angiography (MRA).
- Lifestyle changes: Stop smoking, Control diabetes, Control blood pressure, Be physically active (exercise), Eat a low saturated fat low cholesterol diet.
- Drug Treatment: cilostazol and pentoxifylline.
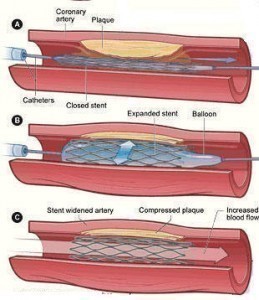
- Angioplasty or Surgery
The prevalence of peripheral vascular disease in people aged over 55 years is 10% -25% and increases with age 70% -80% of affected individuals are asymptomatic, only a minority ever requires revasculation or amputation.
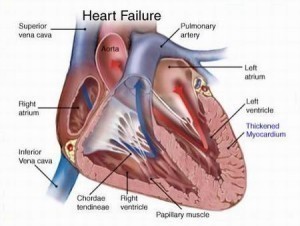
Also, many PVD patients also have angina pectoris or have had myocardial infarction. There is also an increased risk for stroke. The moderate consumption of alcohol has been found to be associated with a reduction of the risk of PVD by almost one third compared to those who do not drink alcohol.
For more information on Peripheral Vascular Disease read: